Introduction:
Antiphospholipid syndrome (APS) is known for its association with unexplained vascular thrombosis and pregnancy-related complications. However, APS can also present with various hematological abnormalities, including thrombocytopenia, autoimmune hemolytic anemia, Evan's syndrome, and thrombotic microangiopathy. While APS is often considered in patients with these manifestations, its laboratory testing yield and patterns in hematology clinics remain underexplored. In this study, we aimed to investigate the prevalence of laboratory positivity for APS in patients attending hematology clinics, even in the absence of meeting the clinical criteria for APS.
Methodology:
This retrospective study was conducted at two tertiary care centers in southern India from January 2018 to June 2023. Patients who visited hematology clinics and underwent APS workup were included. The APS workup involved evaluating Anti Cardiolipin IGG and IGM, Anti Beta2 Glycoprotein IGG and IGM, Lupus Anticoagulant, and ANA. The laboratory criteria for APS were based on the ACR/EULAR APS Criteria. Patients with transiently positive results were excluded from the study. Chi Square test was used for statistical analysis.
Results:
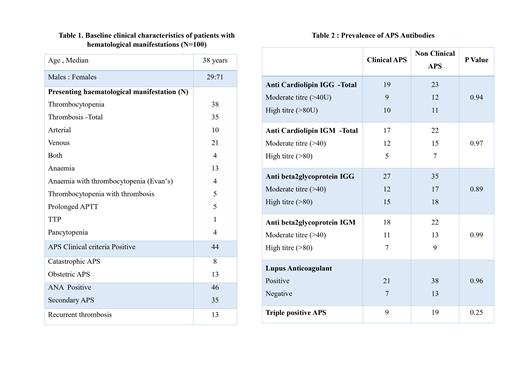
Among the 624 patients who underwent APS workup, 100 patients (16.03%) tested positive for at least one of the laboratory criteria for APS. Remarkably, a significant proportion (56%)of these patients did not fulfill the clinical criteria for APS. The most common hematological manifestations prompting APS testing in these 100 patients were thrombocytopenia (38%) and unprovoked thrombosis (35%). Additional hematological abnormalities included autoimmune hemolytic anemia (13%), prolonged activated partial thromboplastin time (APTT) (5%), Evan's syndrome (4%), pancytopenia (4%), and thrombotic thrombocytopenic purpura (TTP) (1%). Baseline characterstics of our study subjects are shown in Table 1
Anti-beta2 glycoprotein IGG or IGM antibodies were detected in 74% of APS-positive patients, and Anti-cardiolipin IGG or IGM antibodies were found in 57%. Lupus Anticoagulant (LA) was present in 59%. Additionally, 28% of the patients showed positivity for all three antibodies, indicating a significant overlap in laboratory findings. No statistically significant difference in antibody positivity patterns was observed between patients satisfying the clinical criteria for APS and those without, as shown in Table 2
Conclusion:
Our study sheds light on the hematological presentations of APS in patients attending hematology clinics in southern India. Importantly, a substantial number(56%)of patients with APS lab test positivity did not meet the clinical criteria for APS. These findings emphasize the importance of considering APS as a potential diagnosis in patients presenting with hematological manifestations, especially thrombocytopenia and autoimmune hemolytic anemia. Identifying APS in such cases can guide appropriate therapeutic interventions and may help prevent pregnancy-related complications in affected females. Raising awareness among healthcare professionals about the diverse hematological presentations of APS is vital for improving patient outcomes and ensuring timely and accurate diagnoses
Disclosures
No relevant conflicts of interest to declare.